Low Back Pain & Spinal Manipulation – American College of Physicians
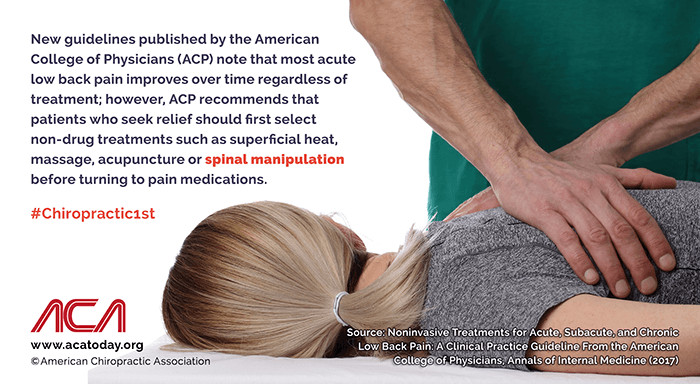
New guidelines published by the American College of Physicians (ACP) note that most acute low back pain improves over time regardless of treatment; however, ACP recommends that patients who seek relief should first select non-drug treatments such as superficial heat, massage, acupuncture or spinal manipulation before turning to pain medications.
Chiropractic Care For Elderly Lower Back Pain

Clear Lake Chiropractor Comments: Chiropractic treatment of elderly lower back pain (LBP) has been reported to be very safe and highly effective. In fact, back in 1994, guidelines were published recommending that chiropractic treatment of low back pain should be a first consideration / treatment of choice in front of many other forms of back care health services. Since that time, more and more studies have been published showing continued advantages of chiropractic care over many other forms of LBP care.
Even though studies have shown that the peak prevalence of LBP occurs in the 5th decade of life, LBP is also a significant public health problem in older adults ranging between 13% and 49% with “…soaring costs in terms of health care expenditures.” So, what about care for the elderly – is chiropractic care equally safe and effective in this older population as it is in younger patients?
A recent study reported two types of spinal manipulation or adjustments verses minimal conservative medical care (MCMC) in patients with subacute or chronic, non-radiating elderly lower back pain over 55 years of age. This included a total of 240 participants, of which 105 were women and 135 were men with an average age of 63 years. The two types of manipulation included a high velocity low amplitude type (the classic “cracking” type of manipulation) and a low velocity variable amplitude type (stretch – not associated with a “crack”) treated 12 times over a 6 week time frame. A 3rd treatment group (MCMC) served as a “control” to compare against the two manipulation approaches. All three groups received a half hour exercise session at week 3 and outcomes were studied at 3, 6, 12 & 24 weeks. The results showed equally effective benefits to the two styles of manipulation over the MCMC group, with no serious adverse events associated with any of the treatment groups.
This study is important in a number of ways. First, it points out that two distinctive styles of manipulation frequently utilized in chiropractic and likely to be encountered by patients obtaining chiropractic care, are equally effective in a population exceeding 55 years of age for elderly lower back pain. The type of manipulation ultimately decided upon can therefore be based on: 1) patient preference (as some patients just don’t like being “cracked”) and 2) the chiropractor’s clinical experience.
When visiting our clinic, we take pride in providing accurate, up-to-date information about our patient’s condition and what must be done to obtain long term, satisfying results. We are most appreciative to have the opportunity to provide care to our patients and strive to make the experience highly satisfying.
If you, a family member or a friend requires care, we sincerely appreciate the trust and confidence shown by choosing our services. We are proud that chiropractic care for elderly lower back pain has consistently scored the highest level of satisfaction when compared to other forms of health care provision and look forward in serving you and your family presently and, in the future.
Dr. Ward Beecher practices at Beecher Chiropractic Clinic at 1001 Pineloch, Ste 700 Houston, TX 77062. You can schedule an appointment at BeecherChiropractic.com or by calling (281) 286-1300. If you have any questions regarding this blog, please comment below!
Can Whiplash Really Happen to YOU?
To download a copy of this week’s newsletter, please click here.
Clear Lake Area Chiropractor Comments: You’re stopped at a red light awaiting a left turn into the grocery store when out of nowhere, you hear the screeching of tires, you turn your head and look into the rear view mirror and see that you’re about to be hit from behind. Then “POW!” The sudden force of the impact propels you back into your seat; your head hits the headrest and then bounces forwards, almost hitting the steering wheel. You feel your body twist due to the angle of the seat belt and your sunglasses fly off and your purse sitting on the seat next to you flies into the dashboard and lands on the floor spilling its contents. You’re not sure what just happened as it all happened so fast. Is this a dream?
Can Whiplash Really Happen?

After collecting yourself and calming down, you get out of the car to inspect the damage and talk to the driver that just ran into you. You notice that right now, you don’t really hurt that much…. but you feel kind of dazed. When you inspect your car, you surprisingly notice very little damage, but it sure felt like your car should be totaled based on the way it felt. The other driver said he was checking the station on the radio and saw you too late. He tried to stop and slammed on the brakes but it was too late. He said, “…I couldn’t have been moving more than 5-10 mph when I hit you!” You ask, “How could this possibly feel so….. hard an impact? Was he lying to me? Do I have Whiplash? Can whiplash really happen?” There certainly wasn’t much damage to your car…maybe he was right??? When he asked you if you would, “…let it go,” and not call the police, you almost agree, but something stops you. Even though there is little car damage and, “…he is a nice guy….,” you just don’t feel right in, “…letting it go.”
Within 15-30 minutes, you’re REALLY HAPPY you didn’t give in and take his advice as by now, your neck is really starting to hurt. You feel kind of nauseated and light headed. Your head is beginning to pound and you feel like you better sit down. When the police officer approaches he seems distant and you’re having difficulty hearing him. Pretty soon, you notice others helping you onto a stretcher and attaching a neck brace prior to taking you to a local emergency room. At the ER, you are confused about the details of the accident but piece together the best you can the events of the evening. They take x-rays, recommend some Advil and ice, and tell you to contact your primary care physician if you have problems. They tell you that you’re going to hurt for a few days and “…that‘s normal.” However, over the next several days, pain intensifies to a point where neck and headache pain is constant, you can’t sleep, your memory seems blurry, you can’t seem to concentrate and loose your place during thought and conversation…. something is REALLY WRONG!
Low Speed Collision Related Injury
This scenario is not atypical of a low speed collision related injury. In fact, the less the car is damaged, the greater the impact is to the contents inside the car (this is called “elastic deformity”). That’s because crushing metal absorbs the energy of the force (ie, “plastic deformity) and if the speed is “…too low” and little metal crushing/energy absorption occurs, the G-forces that occurred during the collision are transferred to the contents inside the vehicle and that force can be significantly greater than a crash that occurs at 2-4 times the 5-10 mph speed. In general, when there is less damage to the car, be alert that the force exerted on the contents is greater than when car damage occurs. This is why when cars crash during a car race, the race car basically falls apart, leaving the driver enclosed in a cage that prevents bodily damage, and they often walk away from the accident.
If you, a loved one, or a friend is struggling with whiplash residuals from a motor vehicle collision, you can depend on receiving an in-depth assessment and therapeutic approach at our chiropractic facility.
Dr. Ward Beecher practices at Beecher Chiropractic Clinic at 1001 Pineloch, Ste 700 Houston, TX 77062. You can schedule an appointment at BeecherChiropractic.com or by calling (281) 286-1300. If you have any questions regarding this blog, please comment below!
Remove Back Pain While Working On A Computer
Duis mollis, est non commodo luctus, nisi erat porttitor ligula, eget lacinia odio sem nec elit. Maecenas sed diam eget risus varius blandit sit amet non magna. Fusce dapibus, tellus ac cursus commodo. Donec ullamcorper nulla non metus.
Benefits Of A Weekly Physiotherapy Session
Duis mollis, est non commodo luctus, nisi erat porttitor ligula, eget lacinia odio sem nec elit. Maecenas sed diam eget risus varius blandit sit amet non magna. Fusce dapibus, tellus ac cursus commodo. Donec ullamcorper nulla non metus.
The Importance of Seatbelts in Auto Accidents
To download a copy of this newsletter, please click here.
Houston Chiropractor Comments: Whiplash is a very common problem afflicting millions of people each year. In fact, there are more than 6 million car accidents each year in the United States alone. Death associated with car accidents occurs every 12 minutes and each year, motor vehicle collisions (MVC) kill 40,000 people. For people aged between 2 and 34 years old, MVCs are the leading cause of death. Another sobering statistic is somebody is injured in a car crash every 14 seconds and about 2 million people receive permanent injuries in car crashes each year. Over a five-year period, over 25% of ALL drivers were involved in a motor vehicle collision. The cost of car accidents averages $1000 for each American per year resulting in a $164.2 billion total cost each year in the United States. Approximately 250,000 children are injured and car crashes, meaning approximately 700 kids are injured daily. Car crashes are the leading cause of acquired disability. Hopefully, these rather startling statistics have gotten your attention.
In general, the available evidence available is clear – seatbelts save lives! Regarding backseat passengers, wearing a seatbelt is 44% more effective at preventing death than riding unrestrained. Similarly, for those positioned in the rear of a van or sport utility vehicle, the use of rear seatbelts is 73% better at preventing a fatal outcome during a car crash. In more than one half of all fatal car accidents, the victims are not properly restrained. In states where rear seatbelts are required, 85% of adult backseat passengers complied versus states not mandating rear seat seatbelt use where only 66% of the passengers complied. The NHTSA has launched a campaign, “Click It or Ticket” and has provided a guide to seatbelt safety promoting the proper use of the seatbelt and have provided the following safety seatbelts tips:
Seatbelt Tips
- Make sure your seat belt fits snugly. Seat belts worn too loosely can cause broken ribs or injuries to your abdomen.
- Place the lap belt low on your hipbones and below your belly. Never put the lap belt across your belly.
- Place the shoulder belt across the center of the chest between the breasts.
- Never slip the upper part of the belt off your shoulder. Seat belts that are worn too high can cause broken ribs or injuries to your belly.
- The most effective safety protection available today for passenger vehicle occupants is lap/shoulder seat belts combined with air bags.
There is a common myth that seatbelts cause injuries at low speeds and therefore, it is better to not wear the seatbelt when simply traveling in your neighborhood. There is overwhelming evidence in almost all circumstances, seatbelts save lives, even at low speed collisions. Because the forces that occur in low-speed crashes are transferred to the contents due to the lack of crushing metal and less vehicle damage, the occupants of a car struck at a low speed can be thrown about significantly… striking the windshield, side window and other contents inside the car. We realize that you have a choice in where you choose for your healthcare services. If you, a friend or family member requires care for whiplash, chiropractic care is a logical first choice and we would be honored to offer our services to you.
Dr. Ward Beecher practices at Beecher Chiropractic Clinic at 1001 Pineloch, Ste 700 Houston, TX 77062. You can schedule an appointment at BeecherChiropractic.com or by calling (281) 286-1300. If you have any questions regarding this blog, please comment below!

Regular Exercise Can Slow Ageing Process
Duis mollis, est non commodo luctus, nisi erat porttitor ligula, eget lacinia odio sem nec elit. Maecenas sed diam eget risus varius blandit sit amet non magna. Fusce dapibus, tellus ac cursus commodo. Donec ullamcorper nulla non metus.
Why You Should See A Physiotherapist After A Fall
Duis mollis, est non commodo luctus, nisi erat porttitor ligula, eget lacinia odio sem nec elit. Maecenas sed diam eget risus varius blandit sit amet non magna. Fusce dapibus, tellus ac cursus commodo. Donec ullamcorper nulla non metus.
What Causes Headaches And What Can I Do About It?
Clear Lake Chiropractor Comments: “I woke up this morning with an excruciating headache. I thought the top of my head was going to blow off!” “I notice as the day goes on, tightness in my neck worsens and I get a headache usually by 2-3pm.” “I don’t know if I can do my work with my headaches.” “What causes headaches like this”?
These are common patient history entries we frequently receive at our clinic. Headaches are one of the most common complaints prompting patients to visit a health care provider. Many patients ask what causes headaches. The National Institutes of Health (NIH) describe the four types of headaches as vascular, muscular contraction or tension, traction and inflammatory.
What Causes Headaches in Common Forms of Headaches
The most common form of a vascular headache is migraine. Migraine sufferers usually complain of severe pain on one or both sides of the head, nausea or vomiting and sometimes visual changes. There is often a heightened sensitivity to light or noise prompting migraine sufferers to lie in a dark, quiet room until the migraine passes. Women are more likely to suffer from migraines than men and the severity of symptoms can be so extreme that all activity must be stopped until it passes.
The next most common type of vascular headache is the toxic headache produced by a fever. Other vascular headache types include “cluster” headaches, which are characterized by repeated episodes of intense pain that start in one spot and spread out from that spot. These may only last a few minutes to an hour but carry a very high level of pain and activity intolerance. Another common type of vascular headache is that resulting from high blood pressure.
Muscle contraction or tension headaches involve tightening of the facial and neck muscles. These often start in the neck and radiate over the top or to the sides of the head. The muscles in the neck are usually extremely tight and tender and often, moderate pressure applied with the finger or thumb to these muscles will prompt radiating pain into and/or over the top of the head. This can also result in significant activity intolerance but usually not as severe as migraine or cluster headaches.
Traction and inflammatory and what causes headaches result because of other conditions that range from a sinus infection to a stroke. These types of headaches can serve as a warning sign of a more significant or serious condition. Another example is meningitis as well as other conditions affecting the sinuses, spine, neck, ear, and teeth.
Preventative Treatment of Headaches
The NIH suggests, when headaches occur ≥3 times a month, that “… preventive treatment is usually recommended.” Certainly, in some cases, medication may be indicated but only after ruling out a more serious condition and after exhausting less invasive treatments that carry fewer side effects.
The American Chiropractic Association recommends: 1) avoid long time periods of staying in one position (computer, sewing machine, reading, etc.) and take stretching/neck range of motion exercise breaks every ½ to 1 hour; 2) Exercise – walking, low impact aerobics; 3) Avoid teeth clenching (due to straining the temporomandibular – TMJ, or jaw joint); 4) Drink lots of water – stay hydrated. These are some of the more common catalysts of what causes headaches.
Chiropractic care may include spinal manipulation (adjustments), nutritional advice (dietary suggestions, vitamin/mineral options such as a B complex), exercise, posture retraining, and relaxation techniques. If you, a family member or a friend require care, we sincerely appreciate the trust and confidence shown by choosing our service. If headaches are a problem, a trial of chiropractic makes sense prior to utilizing a more risk oriented headache treatment option? We look forward in serving you and your family.
Dr. Ward Beecher practices at Beecher Chiropractic Clinic at 1001 Pineloch, Ste 700 Houston, TX 77062. You can schedule an appointment at BeecherChiropractic.com or by calling (281) 286-1300. If you have any questions regarding this blog, please comment below!
20 Exercises You Can Do From Home
Duis mollis, est non commodo luctus, nisi erat porttitor ligula, eget lacinia odio sem nec elit. Maecenas sed diam eget risus varius blandit sit amet non magna. Fusce dapibus, tellus ac cursus commodo. Donec ullamcorper nulla non metus.